Bursa Foot Signs And Symptoms
Retrocalcaneal and retroachilles bursitis are both common types of bursitis that can cause pain at the back of the foot, just above the heel. This pain, and often swelling, occurs when one or both bursae at the back of the heel become irritated and inflamed. Because they have similar symptoms, heel bursitis is sometimes confused with problems affecting the Achilles tendon, which is a long strip of fibrous tissue that connects the back of the heel to the calf muscle. Other times, Achilles tendon problems may bring about the bursitis. For example, tight calf muscles can contribute to chronic pulling where the Achilles tendon inserts into the back of the heel. This pulling can result in friction and irritation that eventually lead to bursitis.
Causes
Repetitive overuse injury of the ankle during long periods of running and or walking. Tight shoes. The heel counter of the shoe constantly rubbing against the back of the heel. Wearing shoes with a low cut heel counter. Abnormal foot mechanics (abnormal pronation). Poor flexibility. Inappropriate training.
Symptoms
Achiness or stiffness in the affected joint. Worse pain when you press on or move the joint. A joint that looks red and swollen (especially when the bursae in the knee or elbow are affected). A joint that feels warm to the touch, compared to the unaffected joint, which could be a sign that you have an infection in the bursa. A ?squishy? feeling when you touch the affected part. Symptoms that rapidly reappear after an injury or sharp blow to the affected area.
Diagnosis
Carrying out a diagnosis for bursitis is fairly straightforward. The doctor will examine the affected area and ask the patient some questions about his/her recent activities. If the patient has a high temperature the physician may take a small sample of fluid from a bursa near the affected body part. The sample will be tested for bacteria, and perhaps also crystals. If the patient does not get better after treatment the doctor may carry out further tests so that he/she can eliminate the possibility that the symptoms might not be due to something else. These may include an x-ray, to make sure no bones are broken or fractured. Blood tests, to check for rheumatoid arthritis. A CT scan or MRI scan to see if there is a torn tendon.
Non Surgical Treatment
In addition to R.I.C.E., there are a number of other treatments to reduce swelling and any associated pain or discomfort due to heel bursitis. Orthotics or change of footwear. Wearing an orthotic device such as a heel insert can encourage better mechanics in the foot and reduce irritation of the retrocalcaneal bursa. Some people do not need special orthotics but simply need to stop wearing shoes with rigid heel and ankle construction and instead wear more supportive, comfortable shoes. Shoes with an "Achilles notch," a groove in the collar at the back of the shoe to protect the Achilles tendon, can be particularly helpful. (Almost all running shoes are designed with an Achilles notch.) Stretching and physical therapy. Stretching the Achilles tendon often helps alleviate pain. Once the pain is resolved it is important for the patient to continue a regular stretching program. Regular stretching reduces the chance of recurrence.
Prevention
You can avoid the situation all together if you stop activity as soon as you see, and feel, the signs. Many runners attempt to push through pain, but ignoring symptoms only leads to more problems. It?s better to take some time off right away than to end up taking far more time off later. Runners aren?t the only ones at risk. The condition can happen to any type of athlete of any age. For all you women out there who love to wear high-heels-you?re at a greater risk as well. Plus, anyone whose shoes are too tight can end up with calcaneal bursitis, so make sure your footwear fits. If the outside of your heel and ankle hurts, calcaneal bursitis could be to blame. Get it checked out.
Recovery From Bunion Hammertoe Surgery
 Overview
Overview
The smallest four toes of each foot have three bony segments connected by two joints. Hammertoe is a deformity in which one or more of the small toes Hammer toes develops a bend at the joint between the first and second segments. The tip of the toe turns downward, making it look like a hammer or claw. The second toe is the one most often affected. Hammer toes may be more likely to occur when the second toe is longer than the first toe or when the arch of the foot is flat.
Causes
Footwear is actually the leading cause of this type of toe deformity so much so that people sometimes require hammer toe surgery to undo some of the damage. The most common problem is wearing shoes that are too short, too narrow or too tight. These shoes constricts the feet and force the toes into a bend position. Women are more at risk especially due to high heels. Footwear isn?t the only problem, poor foot posture can lead to muscle and even bone imbalances. This asymmetry can cause excessive strain on the toes either by forcing the toe into unnatural positions. Arthritis can also play a factor in the development of hammer toe, especially if the toe joint is stiff and incapable of a full range of motion.
 Symptoms
Symptoms
If you have any of these symptoms, do not assume it is due to hammer toe. Talk to your doctor about symptoms such as a toe that curls down, corns on the top of a toe, calluses on the sole of the foot or bottom of the toe, pain in the middle joint of a toe, discomfort on the top of a toe, difficulty finding any shoes that fit comfortably, cramping in a toe, and sometimes also the foot and leg, difficult or painful motion of a toe joint, pain in the ball of the foot or at the base of a toe.
Diagnosis
Your doctor is very likely to be able to diagnose your hammertoe simply by examining your foot. Even before that, he or she will probably ask about your family and personal medical history and evaluate your gait as you walk and the types of shoes you wear. You'll be asked about your symptoms, when they started and when they occur. You may also be asked to flex your toe so that your doctor can get an idea of your range of motion. He or she may order x-rays in order to better define your deformity.
Non Surgical Treatment
Hammertoes that are not painful (asymptomatic) and still flexible may not require treatment. In mild cases, open-toed, low-heeled, or wider shoes and foam or moleskin pads can provide symptomatic relief by reducing pressure. Taping (strapping) the affected toe can help to reduce deformity and pain. Physical therapy to instruct patients in exercises that passively stretch tight structures and strengthen weak foot intrinsic muscles is also helpful with mild cases. Periodic trimming (debridement) of corns (clavi, helomata) by a podiatrist can provide temporary relief. Corticosteroid injections are often very effective in reducing pain.
Surgical Treatment
Until recently, wires were used for surgical correction. In this technique, one or more wires are inserted into the bone through both the affected joint and a normally healthy toe joint, and the end of the toe. These wires stay in place for four to six weeks, protruding from the end of the toes. Due to the protruding wire, simple things such working, driving, bathing and even sleeping are difficult while these wires are in place. During this recovery period, patients often experience discomfort during sleep and are subject possible infection.
Hallux Valgus Treatments
Overview
 Sometimes, the big toe can become angled outwards towards the middle of the foot and second toe. This forces the top of the first metatarsal to stick out from the side of the foot at the base of the big toe. If this happens, the bones can become misaligned and a painful bunion can form. It is not known exactly what causes bunions, but wearing badly fitting shoes is thought to make the condition worse. Research also suggests that bunions may run in families. It is thought that bunions are more likely to occur in people who have unusually flexible joints, and that this flexibility may be inherited. In some cases, certain health conditions, such as rheumatoid arthritis and gout, may also be responsible for the formation of bunions. These conditions cause pain and inflammation in the joints.
Sometimes, the big toe can become angled outwards towards the middle of the foot and second toe. This forces the top of the first metatarsal to stick out from the side of the foot at the base of the big toe. If this happens, the bones can become misaligned and a painful bunion can form. It is not known exactly what causes bunions, but wearing badly fitting shoes is thought to make the condition worse. Research also suggests that bunions may run in families. It is thought that bunions are more likely to occur in people who have unusually flexible joints, and that this flexibility may be inherited. In some cases, certain health conditions, such as rheumatoid arthritis and gout, may also be responsible for the formation of bunions. These conditions cause pain and inflammation in the joints.
Causes
Bunions form when the normal balance of forces that is exerted on the joints and tendons of the foot becomes disrupted. This disruption can lead to instability in the joint and cause the deformity. Bunions are brought about by years of abnormal motion and pressure over the MTP joint. They are, therefore, a symptom of faulty foot development and are usually caused by the way we walk and our inherited foot type or our shoes.
Symptoms
A bony bump along the edge of the foot, at the base of the big toe (adjacent to the ball of the foot) Redness and some swelling at or near the big toe joint. Deep dull pain in the big toe joint. Dull achy pain in the big toe joint after walking or a sharp pain while walking. The big toe is overlapping the second toe, resulting in redness, calluses, or other irritations such as corns.
Diagnosis
The doctor considers a bunion as a possible diagnosis when noting the symptoms described above. The anatomy of the foot, including joint and foot function, is assessed during the examination. Radiographs (X-ray films) of the foot can be helpful to determine the integrity of the joints of the foot and to screen for underlying conditions, such as arthritis or gout. X-ray films are an excellent method of calculating the alignment of the toes when taken in a standing position.
Non Surgical Treatment
Treatment falls into two broad categories, conservative and surgical. From a conservative standpoint, efforts are directed at correcting faulty foot mechanics with custom molded insoles and relief of symptoms. These include Custom Orthosis to stabilize the abnormal motion of the hind and fore foot. Shoe gear modification: Using shoes with larger toe boxed and more supple materials. Changes in activities. Try to avoid those things which cause symptoms. Anti-inflammatory medication for periodic relief this includes cortisone injections into the joint as well as oral medication. 
Surgical Treatment
The choice of surgical procedures (bunionectomy) is based on a biomechanical and radiographic examination of the foot. Because there is actual bone displacement and joint adaptation, most successful bunionectomies require cutting and realigning the 1st metatarsal (an osteotomy). Simply "shaving the bump" is often inadequate in providing long-term relief of symptoms and in some cases can actually cause the bunion to progress faster. The most common procedure performed for the correction of bunions is the 1st metatarsal neck osteotomy, near the level of the joint. This refers to the anatomical site on the 1st metatarsal where the actual bone cut is made. Other procedures are preformed in the shaft of the metatarsal bone (see procedures preformed in the shaft of the metatarsal) and still other procedures are selected by the surgeon that are preformed in the base of the metatarsal bone (see surgeries preformed in the base of the metatarsal).
Prevention
Shop for shoes that possess a removable liner, or insole, and stand on the liner after you have removed it from your shoe. This is an effective method to see if your shoe is wide enough in the forefoot to accommodate your bunion. If your bunion and forefoot are wider than the insole, your shoe will squeeze and constrict your bunion and create the symptoms that define this health problem. The insole should also be wide enough to fully accommodate your big toe when it points outward, away from your other toes.
What Is Overpronation
Overpronation is a term that gets thrown around a lot by psuedo-experts and there is so much written online about it, that it can get very confusing to determine what is legitimate and what is not. Pronation is a normal motion of the foot that occurs when the ankle rolls inwards and the arch collapses. This is normal. Its not something evil. Overpronation is assumed to be when there is too much of it. There certainly is debate as to just how much is too much, as some people have large amounts and have no problems, other have small amounts and do have problems. It all comes down to individual differences and how much force is needed to stop the foot moving. The greater the force, regardless of the amounts of pronation, the more likely it is to be a problem. Some still like to debate if it is a problem or not. Some studies have shown that its not a problem and other studies have shown it is. If the data from all these studies are pooled, then the conclusion was that, yes, overpronation is a problem that was statistically significant, but it was only a small risk factor for problems. An associated finding of overpronation during a gait analysis is an abductory twist.

Causes
There are many causes of flat feet. Obesity, pregnancy or repetitive pounding on a hard surface can weaken the arch leading to over-pronation. Often people with flat feet do not experience discomfort immediately, and some never suffer from any discomfort at all. However, when symptoms develop and become painful, walking becomes awkward and causes increased strain on the feet and calves.
Symptoms
Common conditions seen with overpronation include heel pain or plantar fasciitis, achilles tendonopathy, hallus valgus and or bunions, patellofemoral pain syndrome, Iliotibial band pain syndrome, low back pain, shin splints, stress fractures in the foot or lower leg.
Diagnosis
Pronounced wear on the instep side of shoe heels can indicate overpronation, however it's best to get an accurate assessment. Footbalance retailers offer a free foot analysis to check for overpronation and help you learn more about your feet.

Non Surgical Treatment
Over-Pronation can be treated conservatively (non-surgical treatments) with over-the-counter orthotics. This orthotics should be designed with appropriate arch support and medial rear foot posting to prevent the over-pronation. Footwear should also be examined to ensure there is a proper fit. Footwear with a firm heel counter is often recommended for extra support and stability. Improperly fitting footwear can lead to additional foot problems. If the problem persists, consult your foot doctor.
Surgical Treatment
Hyperpronation can only be properly corrected by internally stabilizing the ankle bone on the hindfoot bones. Several options are available. Extra-Osseous TaloTarsal Stabilization (EOTTS) There are two types of EOTTS procedures. Both are minimally invasive with no cutting or screwing into bone, and therefore have relatively short recovery times. Both are fully reversible should complications arise, such as intolerance to the correction or prolonged pain. However, the risks/benefits and potential candidates vary. Subtalar Arthroereisis. An implant is pushed into the foot to block the excessive motion of the ankle bone. Generally only used in pediatric patients and in combination with other procedures, such as tendon lengthening. Reported removal rates vary from 38% - 100%, depending on manufacturer. HyProCure Implant. A stent is placed into a naturally occurring space between the ankle bone and the heel bone/midfoot bone. The stent realigns the surfaces of the bones, allowing normal joint function. Generally tolerated in both pediatric and adult patients, with or without adjunct soft tissue procedures. Reported removal rates, published in scientific journals vary from 1%-6%.
How You Can Diagnose Calcaneal Apophysitis?
Sever?s disease or Sever?s lesion refers to an injury to the bone growth plate at the back of the heel bone (calcaneous) in young people, particularly those who are physically active. It usually develops in puberty and is slightly more common in boys than girls.
Causes
Physically active children run the risk of developing Sever?s disease because they put the most strain on their growing bones. Sever?s usually occurs during the adolescent growth spurt, when young people grow most rapidly. (This growth spurt can begin any time between the ages of 8 and 13 for girls and 10 and 15 for boys.) By age 15 the back of the heel usually finished growing. As teens grow, the growth plates harden and the growing bones fuse together into mature bone. Young people engaged in physical activities and sports that involve jumping and running on hard surfaces-such as track, basketball, soccer, and gymnastics-are ata higher risk for developing Sever?s disease. Poor-fitting shoes can contribute by not providing enough support or padding for the feet or by rubbing against the back of the heel.
Symptoms
Symptoms of calcaneal apophysitis may include Pain in the back or bottom of the heel, Limping, Walking on toes, Difficulty running, jumping, or participating in usual activities or sports, Pain when the sides of the heel are squeezed.
Diagnosis
Sever?s disease is diagnosed based on a doctor?s physical examination of the lower leg, ankle, and foot. If the diagnosis is in question, the doctor may order x-rays or an MRI to determine if there are other injuries that may be causing the heel pain.
Non Surgical Treatment
Depending on the diagnosis and the severity of the pain, there a number of treatment options available. Rest, reduce activity, your child should reduce or stop any activity that causes pain, such as sports and running. This can be a difficult option, as children are normally quite willful in pursuit of their favorite pastimes. Over the counter anti-inflammatory drugs, such as ibuprofen (found in Nurofen), to help reduce pain and inflammation. Make certain your child does stretching exercises before play. This will often help reduce the stress on the fascia and relieve heel pain in your child. Orthotic insoles. Orthotics made for children will help support the foot properly, and help prevent over-pronation or improper gait by supporting your child?s foot into a proper biomechanical position. Do not hesitate to schedule an appointment with a podiatrist, should your child?s heel and foot pain persist.
Treatment And Cause
Overview
One in four adults in the U.S. has adult acquired flatfoot deformity, which may begin during childhood or be acquired with age. The foot may be flat all the time or may lose its arch when the person stands. The most common and serious cause of flat foot is Posterior Tibial Tendon Dysfunction, in which the main tendon that supports the arch gradually weakens. 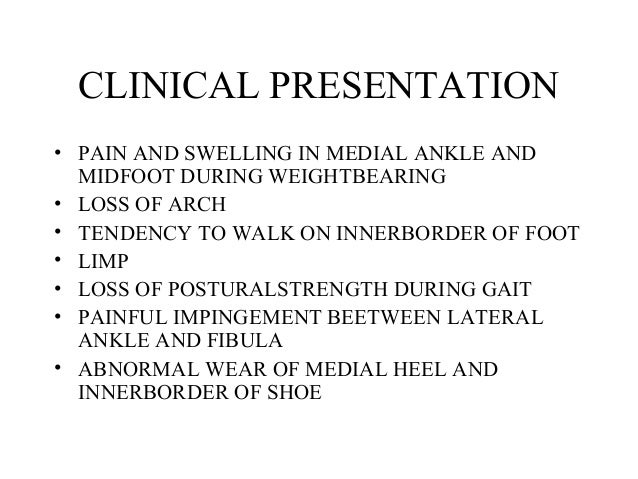
Causes
There are numerous causes of acquired Adult Flatfoot, including, trauma, fracture, dislocation, tendon rupture/partial rupture or inflammation of the tendons, tarsal coalition, arthritis, neuroarthropathy and neurologic weakness. The most common cause of acquired Adult Flatfoot is due to overuse of a tendon on the inside of the ankle called the posterior tibial tendon. This is classed as - posterior tibial tendon dysfunction. What are the causes of Adult Acquired flat foot? Trauma, Fracture or dislocation. Tendon rupture, partial tear or inflammation. Tarsal Coalition. Arthritis. Neuroarthropathy. Neurological weakness.
Symptoms
Patients will usually describe their initial symptoms as "ankle pain", as the PT Tendon becomes painful around the inside of the ankle joint. The pain will become more intense as the foot flattens out, due to the continued stretching and tearing of the PT Tendon. As the arches continue to fall, and pronation increases, the heel bone (Calcaneus) tilts into a position where it pinches against the ankle bone (Fibula), causing pain on both the inside and outside of the ankle. As the foot spends increased time in a flattened, or deformed position, Arthritis can begin to affect the joints of the foot, causing additional pain.
Diagnosis
Although you can do the "wet test" at home, a thorough examination by a doctor will be needed to identify why the flatfoot developed. Possible causes include a congenital abnormality, a bone fracture or dislocation, a torn or stretched tendon, arthritis or neurologic weakness. For example, an inability to rise up on your toes while standing on the affected foot may indicate damage to the posterior tibial tendon (PTT), which supports the heel and forms the arch. If "too many toes" show on the outside of your foot when the doctor views you from the rear, your shinbone (tibia) may be sliding off the anklebone (talus), another indicator of damage to the PTT. Be sure to wear your regular shoes to the examination. An irregular wear pattern on the bottom of the shoe is another indicator of acquired adult flatfoot. Your physician may request X-rays to see how the bones of your feet are aligned. Muscle and tendon strength are tested by asking you to move the foot while the doctor holds it.
Non surgical Treatment
A painless flatfoot that does not hinder your ability to walk or wear shoes requires no special treatment or orthotic device. Other treatment options depend on the cause and progression of the flatfoot. Conservative treatment options include making shoe modifications. Using orthotic devices such as arch supports and custom-made orthoses. Taking nonsteroidal anti-inflammatory drugs such as ibuprofen to relieve pain. Using a short-leg walking cast or wearing a brace. Injecting a corticosteroid into the joint to relieve pain. Rest and ice. Physical therapy. In some cases, surgery may be needed to correct the problem. Surgical procedures can help reduce pain and improve bone alignment. 
Surgical Treatment
Surgical correction is dependent on the severity of symptoms and the stage of deformity. The goals of surgery are to create a more functional and stable foot. There are multiple procedures available to the surgeon and it may take several to correct a flatfoot deformity. Usually surgical treatment begins with removal of inflammatory tissue and repair of the posterior tibial tendon. A tendon transfer is performed if the posterior tibial muscle is weak or the tendon is badly damaged. The most commonly used tendon is the flexor digitorum longus tendon. This tendon flexes or moves the lesser toes downward. The flexor digitorum longus tendon is utilized due to its close proximity to the posterior tibial tendon and because there are minimal side effects with its loss. The remainder of the tendon is sutured to the flexor hallucis longus tendon that flexes the big toe so that little function is loss.
Pain In The Arches All You Need To Know
Flexible flatfeet are considered normal in young children because babies are not born with a normal arch. The arch may not form fully until sometime between ages 7 and 10. Even in adulthood, 15% to 25% of people have flexible flatfeet. Most of these people never develop symptoms. In many adults who have had flexible flatfeet since childhood, the missing arch is an inherited condition related to a general looseness of ligaments. These people usually have extremely flexible, very mobile joints throughout the body, not only in the feet. Flatfeet also can develop during adulthood. Causes include joint disease, such as rheumatoid arthritis, and disorders of nerve function (neuropathy).

Causes
A common cause of foot arch pain is a stress fracture. They tend to occur from repeated overloading of one of the foot bones from activities such as jumping and running especially if you have suddenly increased your activity level. The breaks in the bone may be small but they can be extremely painful. Stress fractures of the metatarsal bones or the navicular can cause anything from mild to severe foot arch pain. The Tibialis Posterior muscle plays a very important role in supporting the medial arch of the foot. Posterior Tibial Tendonitis can occur either through repetitive use e.g. high impact sports such as soccer or tennis, or from an injury e.g. a fall. This causes the tendon to become inflamed or even torn, resulting in pain on bottom of foot. This pain usually gets worse with activity or when standing for long periods. If the problem persists, the inner side of the foot (known as the medial longitudinal arch of the foot) gradually collapses down, causing flat feet. A simple test for this condition is to stand on one leg and rise up onto your tiptoes. If you cannot, it indicates a problem with the Posterior Tibial tendon. Treatment usually consists of rest, ice, exercises, orthotics and physical therapy.
Symptoms
Repetitive exertive activity arch pain is usually sharp, and localized to a specific area, rather than the entire arch. Usually the pain occurs in the area just in front of the heel. It is present when first standing on the foot in the morning, but may decrease once you start walking around, but will, gradually becomes worse with continued walking or running. Swelling may be present. The pain subsides with rest, but stretching the arch while resting may cause the pain to return. Injury pain is constantly present, but worse when standing on the foot. This pain is localized to a specific area, but may radiate out from this area to the entire foot. The pain is sharp, and usually accompanied by swelling and occasionally "black and blue" discolorations. The pain due to the natural aging process is usually dull and aching, or stiff, and can be felt throughout the entire arch area, rather then in just one spot. This pain is present whenever weight bearing, and usually becomes worse with continued walking. The pain gradually subsides when resting, and usually does not return with stretching. Biomechanical defect pain is usually localized to a section of the arch, such as the inner, middle, outer, front, or back of the arch. This pain may be sharp or dull, but is always worse with continued walking.
Diagnosis
To come to a correct diagnosis, your podiatrist will examine your foot by using his or her fingers to look for a lump or stone bruise in the ball of your foot. He or she will examine your foot to look for deformities such as high or low arches, or to see if you have hammertoes. He or she may use x-rays, MRIs (magnetic resource imaging), and CT scans to rule out fractures and damage to ligaments, tendons, and other surrounding tissues. Your doctor will also inquire about your daily activities, symptoms, medical history, and family history. If you spend a lot of time running or jumping, you may be at a higher risk for pain in the bottom of your foot. These diagnostic tests will help your doctor come to a proper diagnosis and create an appropriate treatment plan.
Non Surgical Treatment
Stretch the fascia. Prop your toes up against a wall, keeping your arch and heel flat so the toes stretch. Hold for a count of 10. Repeat 10 times three or four times per day. Roll a frozen water bottle under the arch. Stretch first then roll out the arch for 10 minutes; you don?t want to stretch the tendon when it?s ice cold. Freeze a golf ball and massage the fascia. Roll the frozen golf ball under the foot, starting from the front and working your way back. Put good pressure on each spot-the medial, center and lateral positions-for 15 seconds before moving to the next area. Then, roll the ball back and forth over the entire foot. Foam roll all muscles on the body above the plantar. Even tight shoulders can cause the condition, as your arm swing can throw off proper hip alignment and footstrike. Bump your arch. Get a commercial insole with an arch bump to push on the plantar and keep it from flexing-it doesn?t matter if you?re an under or overpronator; the plantar needs to be supported and strengthened, Wear the support in all shoes, if possible.

Surgical Treatment
The main goal of surgery is to reduce pain and improve function. It may also reduce other injuries such as repeated ankle sprains and broken bones. Surgery may be considered if there is no relief with physical therapy, changes in shoewear and/or changes in activity. Some patients will also have tendon problems, ankle weakness and foot fractures. These patients may require other procedures to address related problems. If you have medical problems that make surgery unsafe, any infections or blood vessel disease, cavus foot surgery may not be appropriate. The surgical procedures involved with the correction of the cavus foot are varied. Theses may include correction of the bony deformity, ankle looseness and the muscle imbalances that cause the deformity. The goal is to provide a foot that evenly distributes weight along both inside and outside edges. A variety of incisions may be needed to perform the procedures related to the correction of the cavus foot.
Prevention
Stretch and strengthen important muscles in your feet, ankles and legs in order to guard against future strain. Make sure to acquire suitable arch supports and inserts if necessary, and that your shoes are shock absorbent and in good condition. Wearing tattered shoes provides no protection, and runners should replace their footwear before exceeding 500 miles of usage. Athletes new to arch supports should gradually build their training routine, allowing their feet to become accustomed to a new stance.