Posterior Tibial Tendon Dysfunction (PTTD)
Overview
Posterior tibial tendon dysfunction (PTTD) is an inflammation and / or overstretching of the posterior tibial tendon in the foot. An important function of the posterior tibial tendon is to help support the arch. But in PTTD, the tendon?s ability to perform that job is impaired, often resulting in a flattening of the foot. PTTD is often called ?adult-acquired flatfoot? because it is the most common type of flatfoot developed during adulthood. Although this condition typically occurs in only one foot, some people may develop it in both feet. PTTD is usually progressive, which means it will keep getting worse-especially if it isn?t treated early. This differs from flexible flatfoot because flexible flatfoot typically begins in childhood or adolescence and continues into adulthood. It usually occurs in both feet and generally progresses in severity throughout the adult years. As the deformity worsens, the soft tissues (tendons and ligaments) of the arch may stretch or tear and become inflamed. The term ?flexible? means that while the foot is flat when standing (weight bearing), the arch returns when not standing. In the early stages of flexible flatfoot arthritis is not restricting motion of the arch and foot, but in the later stages arthritis may develop to such a point that the arch and foot become stiff. 
Causes
The most common cause of acquired adult flatfoot is posterior tibial tendon dysfunction. What causes adult acquired flat foot? Fracture or dislocation. Tendon laceration. Tarsal Coalition. Arthritis. Neuroarthropathy. Neurological weakness.
Symptoms
In many cases, adult flatfoot causes no pain or problems. In others, pain may be severe. Many people experience aching pain in the heel and arch and swelling along the inner side of the foot.
Diagnosis
Examination by your foot and ankle specialist can confirm the diagnosis for most patients. An ultrasound exam performed in the office setting can evaluate the status of the posterior tibial tendon, the tendon which is primarily responsible for supporting the arch structure of the foot.
Non surgical Treatment
Because of the progressive nature of PTTD, early treatment is advised. If treated early enough, your symptoms may resolve without the need for surgery and progression of your condition can be arrested. In contrast, untreated PTTD could leave you with an extremely flat foot, painful arthritis in the foot and ankle, and increasing limitations on walking, running, or other activities. In many cases of PTTD, treatment can begin with non-surgical approaches that may include orthotic devices or bracing. To give your arch the support it needs, your foot and ankle surgeon may provide you with an ankle brace or a custom orthotic device that fits into the shoe. Immobilization. Sometimes a short-leg cast or boot is worn to immobilize the foot and allow the tendon to heal, or you may need to completely avoid all weight-bearing for a while. Physical therapy. Ultrasound therapy and exercises may help rehabilitate the tendon and muscle following immobilization. Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Shoe modifications. Your foot and ankle surgeon may advise changes to make with your shoes and may provide special inserts designed to improve arch support.
Surgical Treatment
If conservative treatment fails to provide relief of pain and disability then surgery is considered. Numerous factors determine whether a patient is a surgical candidate. They include age, obesity, diabetes, vascular status, and the ability to be compliant with post-operative care. Surgery usually requires a prolonged period of nonweightbearing immobilization. Total recovery ranges from 3 months to one year. Clinical, x-ray, and MRI examination are all used to select the appropriate surgical procedure.
Treating Flat Feet In Adults
Overview
Most flat feet are not painful, particularly those flat feet seen in children. In the adult acquired flatfoot, pain occurs because soft tissues (tendons and ligaments) have been torn. The deformity progresses or worsens because once the vital ligaments and posterior tibial tendon are lost, nothing can take their place to hold up the arch of the foot. The painful, progressive adult acquired flatfoot affects women four times as frequently as men. It occurs in middle to older age people with a mean age of 60 years. Most people who develop the condition already have flat feet. A change occurs in one foot where the arch begins to flatten more than before, with pain and swelling developing on the inside of the ankle. Why this event occurs in some people (female more than male) and only in one foot remains poorly understood. Contributing factors increasing the risk of adult acquired flatfoot are diabetes, hypertension, and obesity. 
Causes
There are numerous causes of acquired Adult Flatfoot, including, trauma, fracture, dislocation, tendon rupture/partial rupture or inflammation of the tendons, tarsal coalition, arthritis, neuroarthropathy and neurologic weakness. The most common cause of acquired Adult Flatfoot is due to overuse of a tendon on the inside of the ankle called the posterior tibial tendon. This is classed as - posterior tibial tendon dysfunction. What are the causes of Adult Acquired flat foot? Trauma, Fracture or dislocation. Tendon rupture, partial tear or inflammation. Tarsal Coalition. Arthritis. Neuroarthropathy. Neurological weakness.
Symptoms
The first stage represents inflammation and symptoms originating from an irritated posterior tibial tendon, which is still functional. Stage two is characterized by a change in the alignment of the foot noted on observation while standing (see above photos). The deformity is supple meaning the foot is freely movable and a ?normal? position can be restored by the examiner. Stage two is also associated with the inability to perform a single-leg heel rise. The third stage is dysfunction of the posterior tibial tendon is a flatfoot deformity that becomes stiff because of arthritis. Prolonged deformity causes irritation to the involved joints resulting in arthritis. The fourth phase is a flatfoot deformity either supple (stage two) or stiff (stage 3) with involvement of the ankle joint. This occurs when the deltoid ligament, the major supporting structure on the inside of the ankle, fails to provide support. The ankle becomes unstable and will demonstrate a tilted appearance on X-ray. Failure of the deltoid ligament results from an inward displacement of the weight bearing forces. When prolonged, this change can lead to ankle arthritis. The vast majority of patients with acquired adult flatfoot deformity are stage 2 by the time they seek treatment from a physician.
Diagnosis
Perform a structural assessment of the foot and ankle. Check the ankle for alignment and position. When it comes to patients with severe PTTD, the deltoid has failed, causing an instability of the ankle and possible valgus of the ankle. This is a rare and difficult problem to address. However, if one misses it, it can lead to dire consequences and potential surgical failure. Check the heel alignment and position of the heel both loaded and during varus/valgus stress. Compare range of motion of the heel to the normal contralateral limb. Check alignment of the midtarsal joint for collapse and lateral deviation. Noting the level of lateral deviation in comparison to the contralateral limb is critical for surgical planning. Check midfoot alignment of the naviculocuneiform joints and metatarsocuneiform joints both for sag and hypermobility.
Non surgical Treatment
Get treated early. There is no recommended home treatment. While in stage one of the deformity, rest, a cast, and anti-inflammatory therapy can help you find relief. This treatment is followed by creating custom-molded foot orthoses and orthopedic footwear. These customized items are critical in maintaining the stability of the foot and ankle. Once the tendon has stretched and deformity is visible, the chances of success for non-surgical treatment are significantly lower. In a small percentage of patients, total immobilization may arrest the progression of the deformity. A long-term brace known as an ankle foot orthosis is required to keep the deformity from progressing. The Richie Brace, a type of ankle foot orthosis, shows significant success as a treatment for stage two posterior tibial dysfunction. It is a sport-style brace connected to a custom corrected foot orthodic that fits into most lace-up footwear (including athletic shoes). It is also light weight and more cosmetically appealing than traditionally prescribed ankle foot orthosis. The Arizona Brace, California Brace or Gauntlet Brace may also be recommended depending on your needs. 
Surgical Treatment
Surgery should only be done if the pain does not get better after a few months of conservative treatment. The type of surgery depends on the stage of the PTTD disease. It it also dictated by where tendonitis is located and how much the tendon is damaged. Surgical reconstruction can be extremely complex. Some of the common surgeries include. Tenosynovectomy, removing the inflamed tendon sheath around the PTT. Tendon Transfer, to augment the function of the diseased posterior tibial tendon with a neighbouring tendon. Calcaneo-osteotomy, sometimes the heel bone needs to be corrected to get a better heel bone alignment. Fusion of the Joints, if osteoarthritis of the foot has set in, fusion of the joints may be necessary.
Insertional Achilles Tendonitis Massage
 Achilles tendinitis is an irritation/inflammation in the achilles tendon, which attaches to the back of the heel. It is often a result of overuse and occurs frequently in runners who have altered their training suddenly, either with regard to duration or intensity. This injury is also prevalent in middle-aged people who are active.
Achilles tendinitis is an irritation/inflammation in the achilles tendon, which attaches to the back of the heel. It is often a result of overuse and occurs frequently in runners who have altered their training suddenly, either with regard to duration or intensity. This injury is also prevalent in middle-aged people who are active.
Causes
There are a number of ways a person can develop Achilles tendinitis. Some causes are easier to avoid than others, but being aware of them can aid earlier diagnosis and help prevent serious injury. Causes of Achilles tendinitis include, using incorrect or worn out shoes when running or exercising. Not warming up properly before exercise. Increasing intensity of exercise too quickly (e.g. running speed or distance covered). Prematurely introducing hill running or stair climbing to exercise routine. Running on hard or uneven surfaces. Calf muscle is injured or has little flexibility (this puts a lot of strain on the Achilles tendon). Sudden intense physical activity such as sprinting for the finish line. Achilles tendinitis can also be caused by differences in foot, leg or ankle anatomy. For example, some people can have flatness in their foot where there would normally be an arch; this puts more strain on the tendon. The FDA has asked that a boxed warning be added to the prescribing information for fluoroquinolone antibiotics. Patients taking these drugs may experience an increased risk of tendinitis and tendon rupture. Fluoroquinolones include Cipro (ciprofloxacin), Factive (gemifloxacin), Levaquin (levofloxacin), Avelox (moxifloxacin), Noroxin (norfloxacin), Floxin (ofloxacin) and Proquin (ciprofloxacin hydrochloride). It is important to remember that the risk for injury is not necessarily gone when the drug is stopped. Cases have been reported in which tendon problems occurred up to several months after the drug was discontinued.
Symptoms
Symptoms of Achilles tendinitis and tendinosis include recurring localized heel pain, sometimes severe, along the achilles tendon during or after exercise. Pain often begins after exercise and gradually worsens. Morning tenderness or stiffness about an inch and a half above the point where the Achilles tendon is attached to the heel bone. Sluggishness in your leg. Mild to severe swelling. Stiffness that generally diminishes as the tendon warms up with use.
Diagnosis
Studies such as x-rays and MRIs are not usually needed to make the diagnosis of tendonitis. While they are not needed for diagnosis of tendonitis, x-rays may be performed to ensure there is no other problem, such as a fracture, that could be causing the symptoms of pain and swelling. X-rays may show evidence of swelling around the tendon. MRIs are also good tests identify swelling, and will show evidence of tendonitis. However, these tests are not usually needed to confirm the diagnosis; MRIs are usually only performed if there is a suspicion of another problem that could be causing the symptoms. Once the diagnosis of tendonitis is confirmed, the next step is to proceed with appropriate treatment. Treatment depends on the specific type of tendonitis. Once the specific diagnosis is confirmed, the appropriate treatment of tendonitis can be initiated.
Nonsurgical Treatment
Most of the time, treatment for achilles tendinitis beginning with nonsurgical options. Your CFO physician may recommend rest, ice, ibuprofen, and physical therapy. If after 6 months, the pain does not improve, surgical treatment may be necessary. The type of surgery would depend on the exact location of the tendinitis and extent of damage.

Surgical Treatment
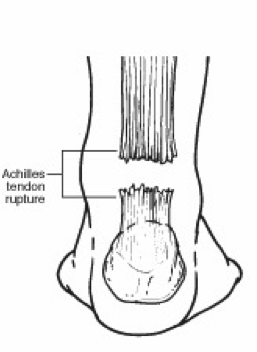
Surgery for an Achilles tendon rupture can be done with a single large incision, which is called open surgery. Or it can be done with several small incisions. This is called percutaneous surgery. The differences in age and activity levels of people who get surgery can make it hard to know if Achilles tendon surgery is effective. The success of your surgery can depend on, your surgeon's experience. The type of surgery you have. How damaged the tendon is. How soon after rupture the surgery is done. How soon you start your rehab program after surgery. How well you follow your rehab program. Talk to your surgeon about his or her surgical experience. Ask about his or her success rate with the technique that would best treat your condition.
Prevention
Achilles tendinitis cannot always be prevented but the following tips will help you reduce your risk. If you are new to a sport, gradually ramp up your activity level to your desired intensity and duration. If you experience pain while exercising, stop. Avoid strenuous activity that puts excessive stress on your Achilles tendon. If you have a demanding workout planned, warm up slowly and thoroughly. Always exercise in shoes that are in good condition and appropriate for your activity or sport. Be sure to stretch your calf muscles and Achilles tendon before and after working out. If you suffer from Achilles tendinitis make sure you treat it properly and promptly. If self-care techniques don?t work, don?t delay. Book a consultation with a foot care expert or you may find yourself sidelined from your favourite sports and activities.